Shape my smile Additive approach using biometrics
Dario Novak specialises in minimally invasive aesthetic dentistry. In this article he documents step by step the “Shape my smile” workflow using biometric design combined with the injectable mould technique for direct restorations. Read his story below.
Is this going to damage my tooth? This is the second question I hear from almost each of my patients on a daily basis, regardless of the procedure in question. Whether it is changing a filling, sandblasting after tartar removal, or even bleaching. The “age of Information” revolutionised the way we think and work, but one side effect is also the fact that our patients are even more opinionated and all-knowing. The main fear they have is basically unnecessary prepping of the teeth, even when we have a clear clinical indication to do so. Basically we live in an era where information, curated or not, permanently distorts the patient’s ability to trust his doctor and his indications. “Non-invasive” is a blessing from our point of view, but a well established curse as well.
Mittigating modern curses with modern tools
Shape my smile is a completely digitalised, minimally invasive additive approach for restoring esthetics and function using natural teeth libraries in the design process and transferring it using an injectable mould technique.
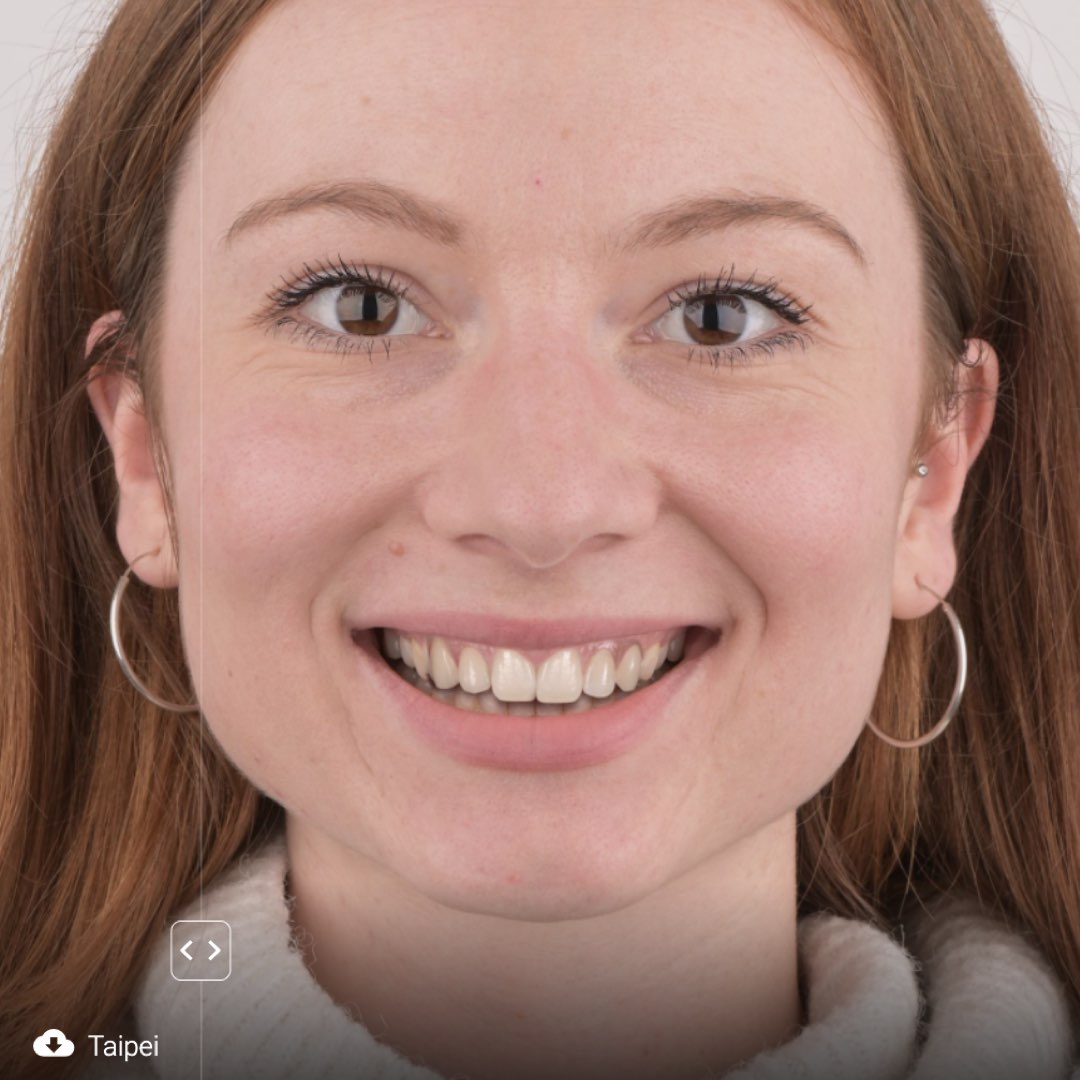
Meet Dina.




Design process




Recognising the indication
What makes a case purely additive?
- Multiple diastemas
- Post-ortho patients
- Missing tooth structure (if the function is preserved)
- Lack of aesthetic tooth display
- Overall correction of anterior tooth display

Contraindications
- Color changing indication (one or all of the teeth have unpleasant color for the patient and his main complaint is to change the color of the teeth)
- Crowding
- Cases that would need reduction of tooth structure
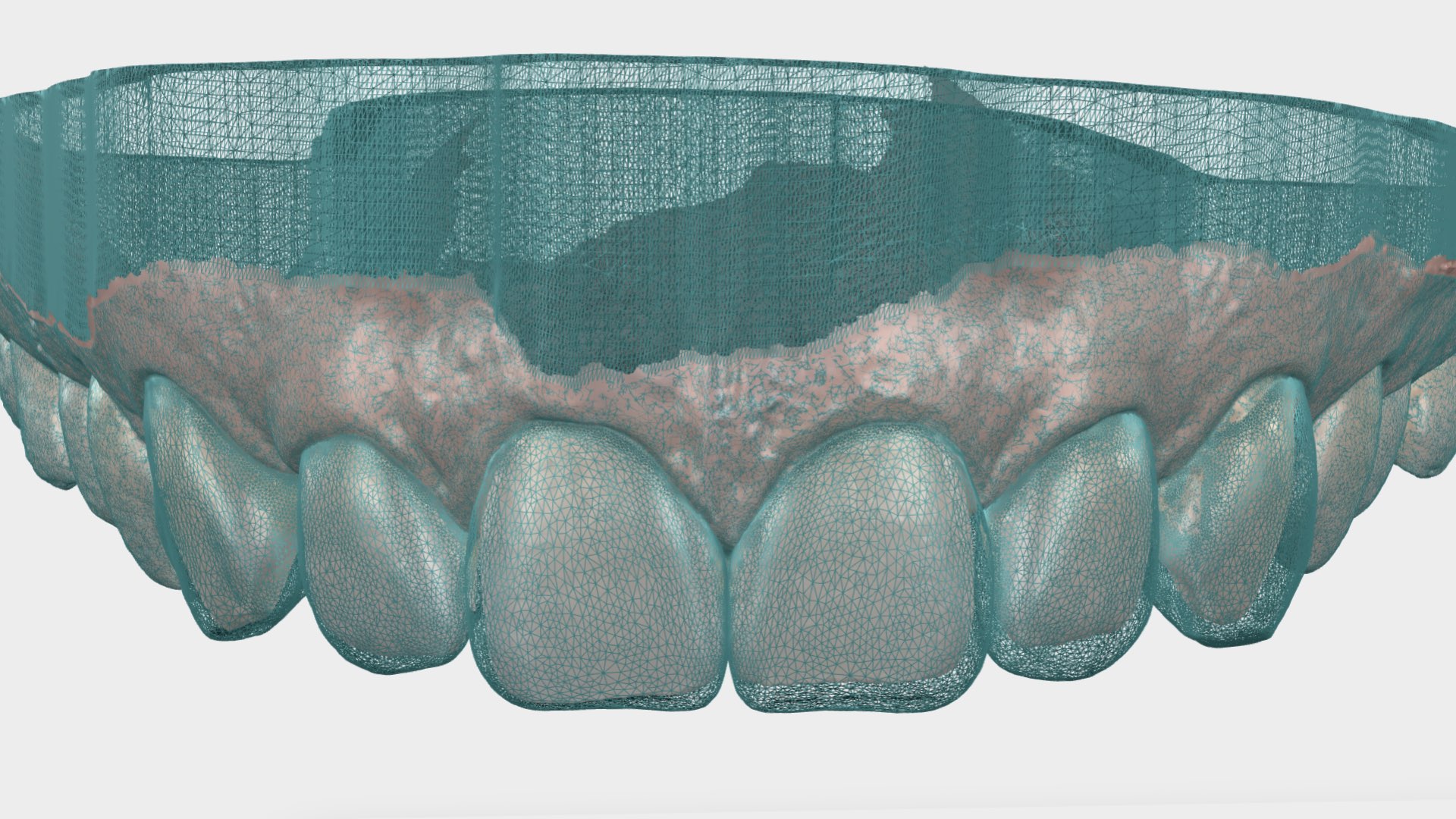
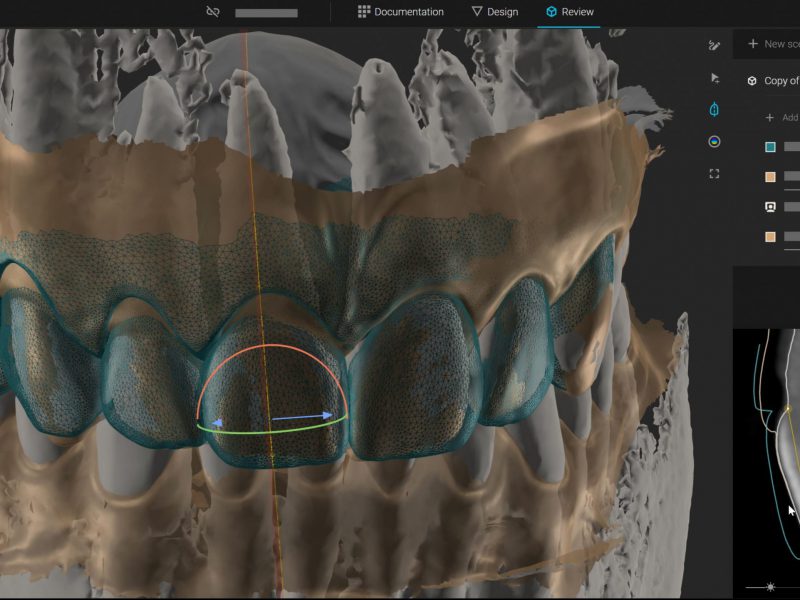
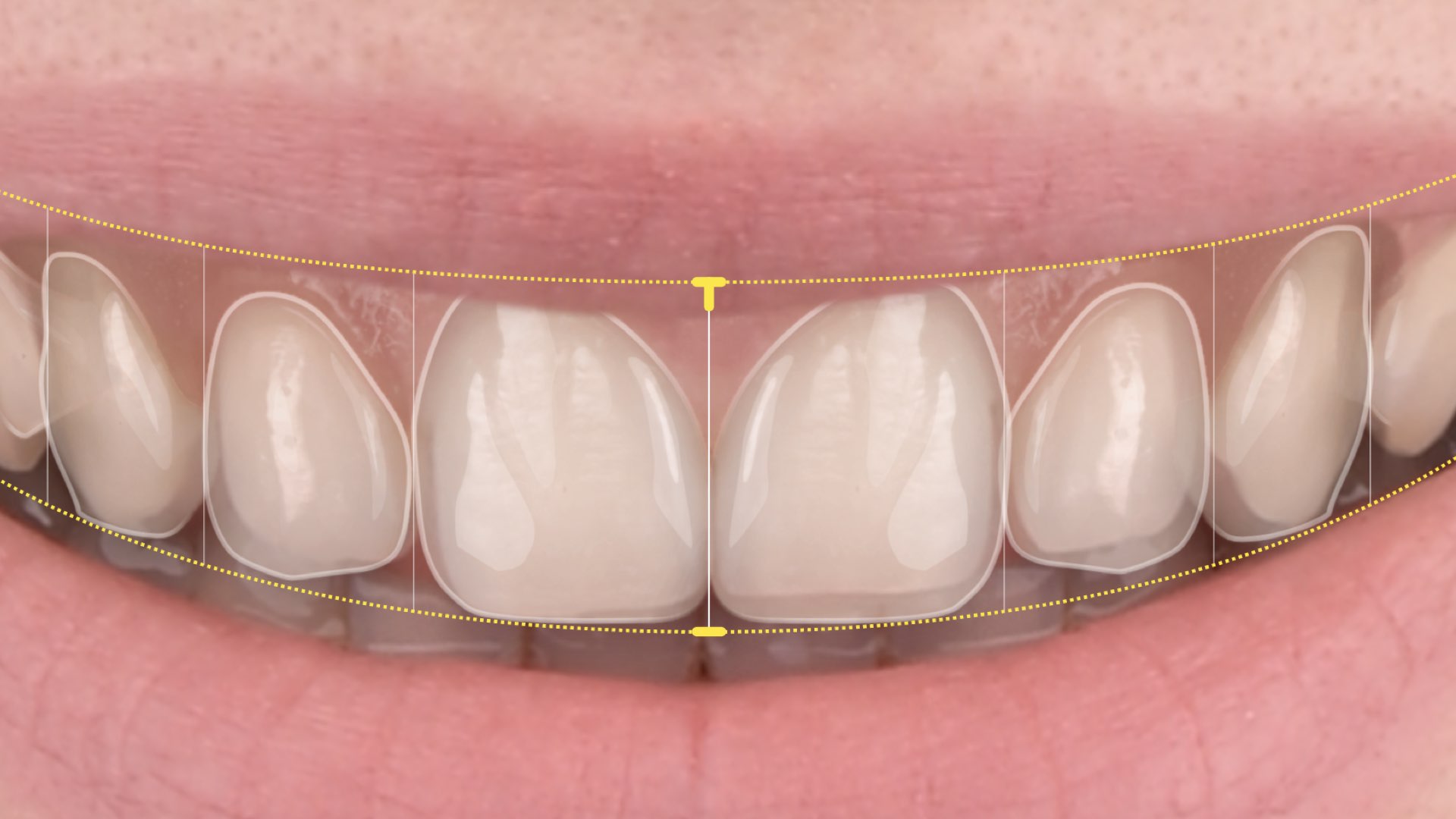
Transforming 2D into 3D
Technical bottlenecks


Assessing thickness
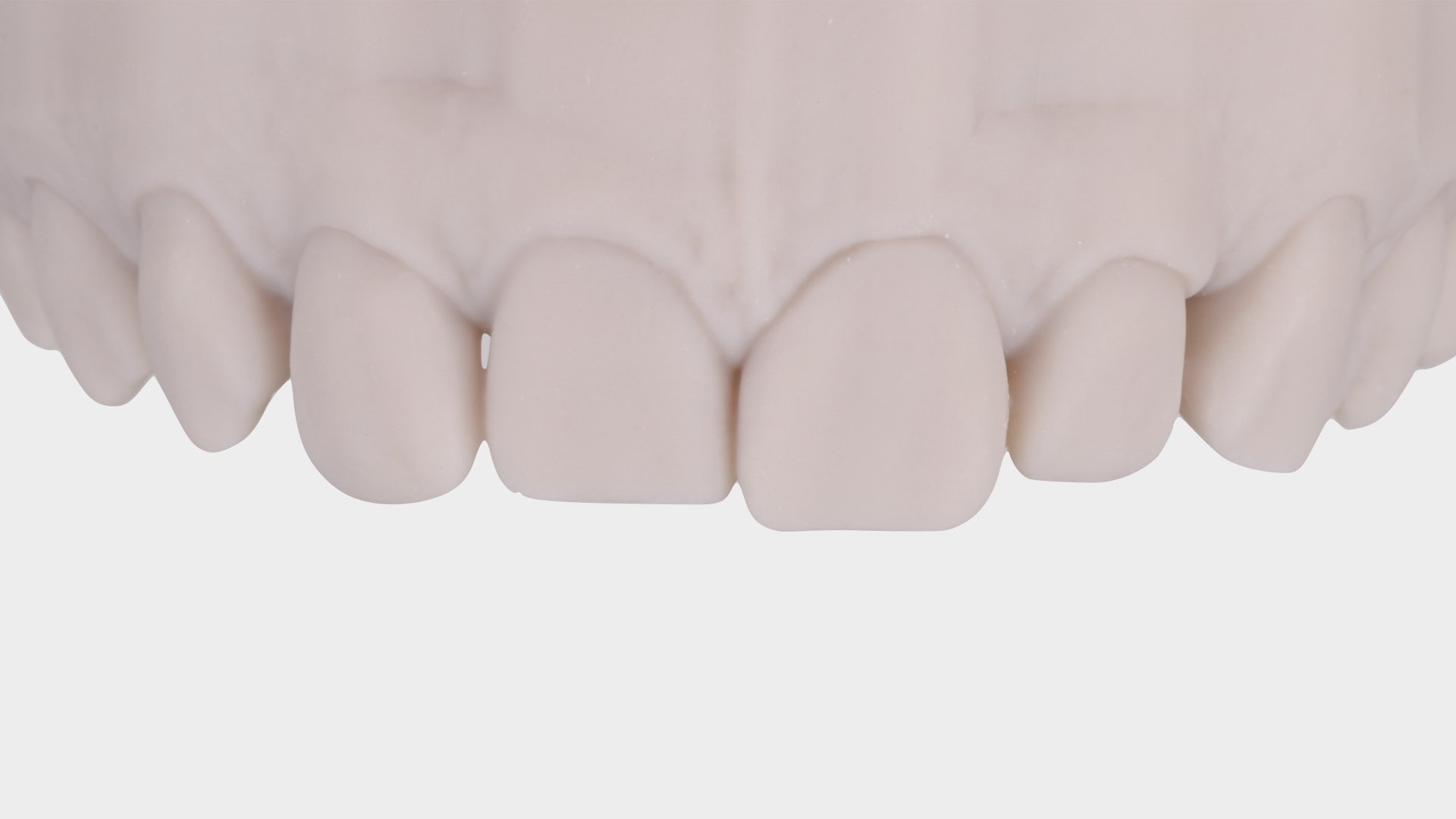
Final mockup

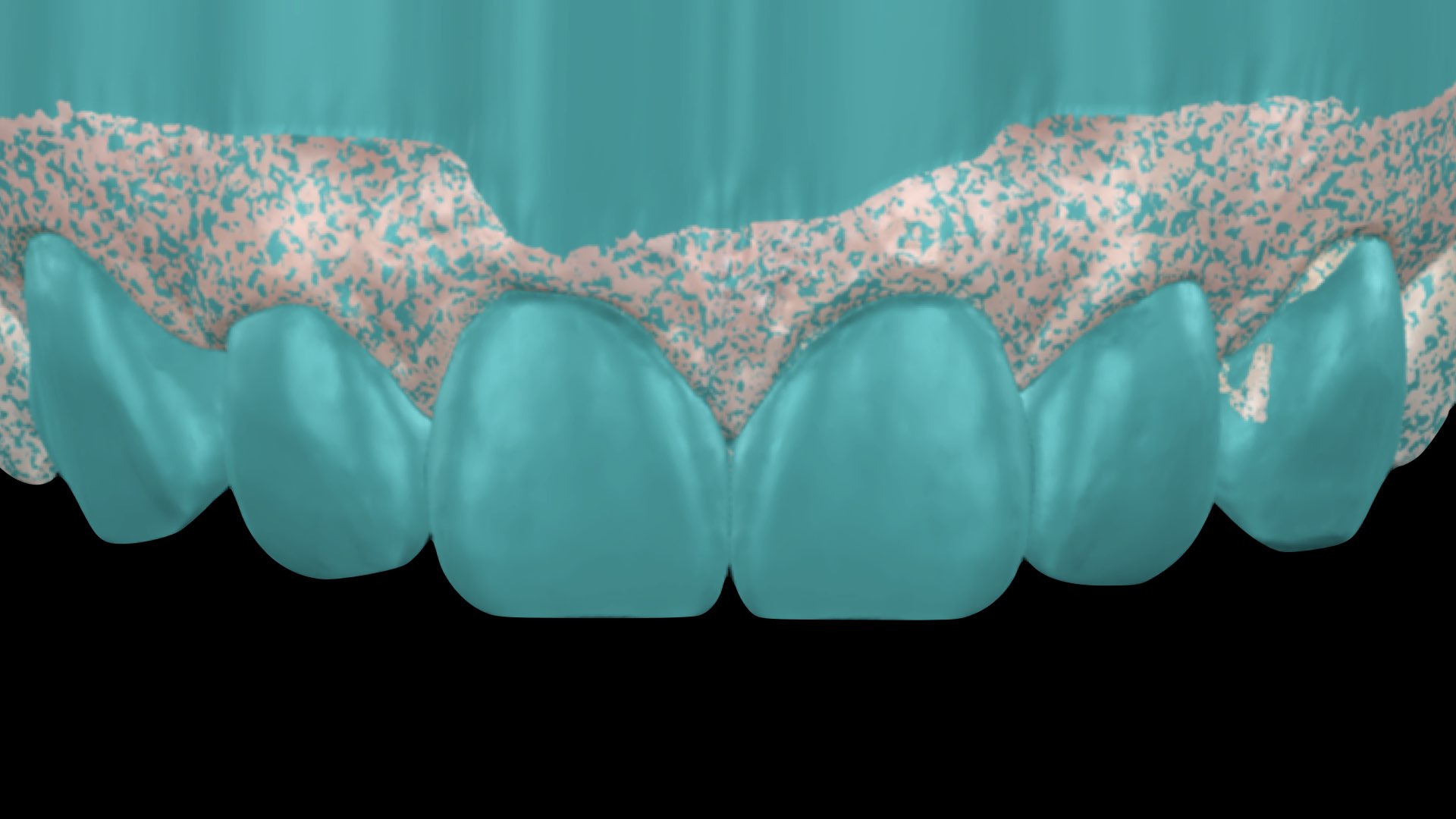
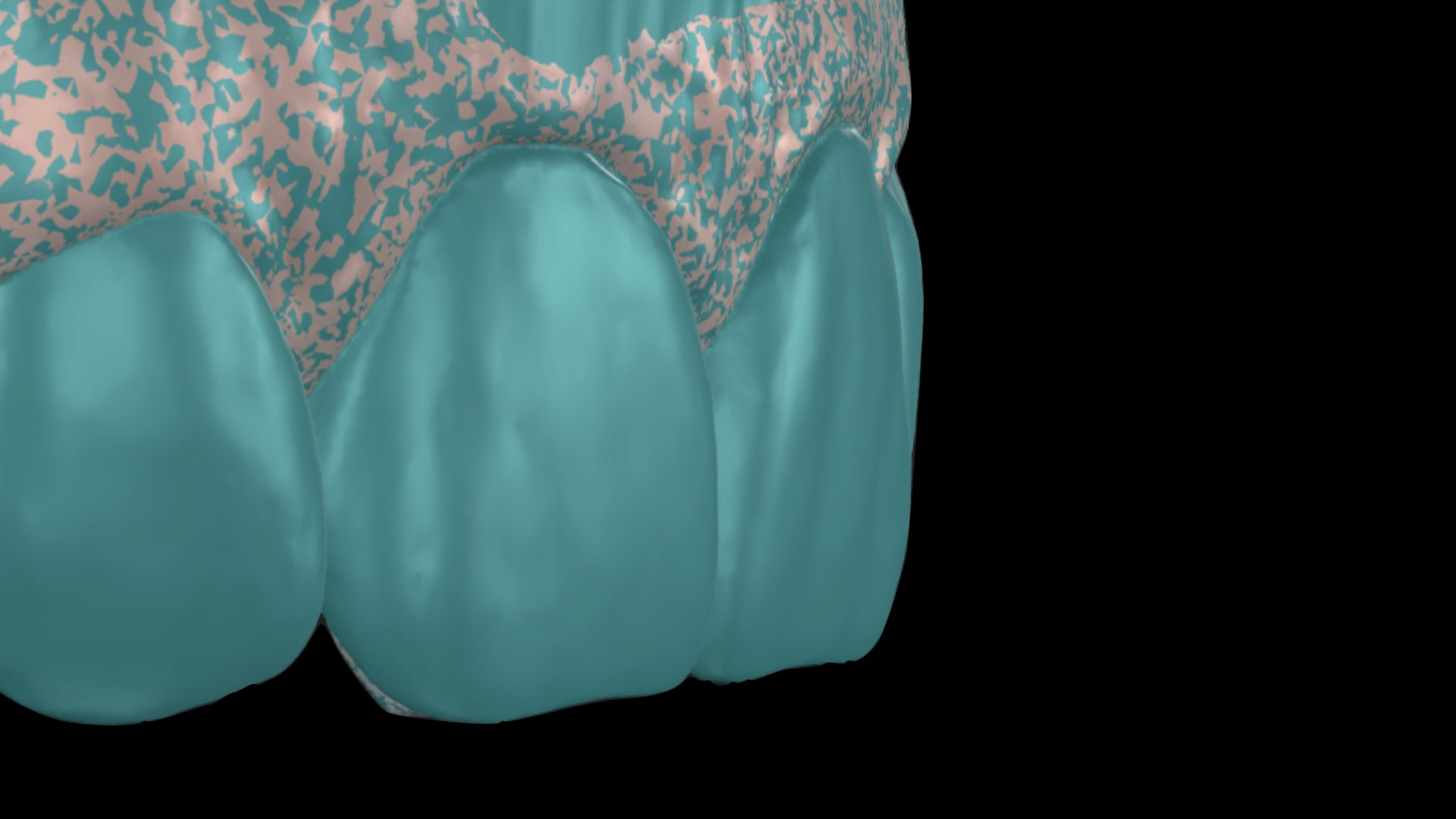
Transparent mould

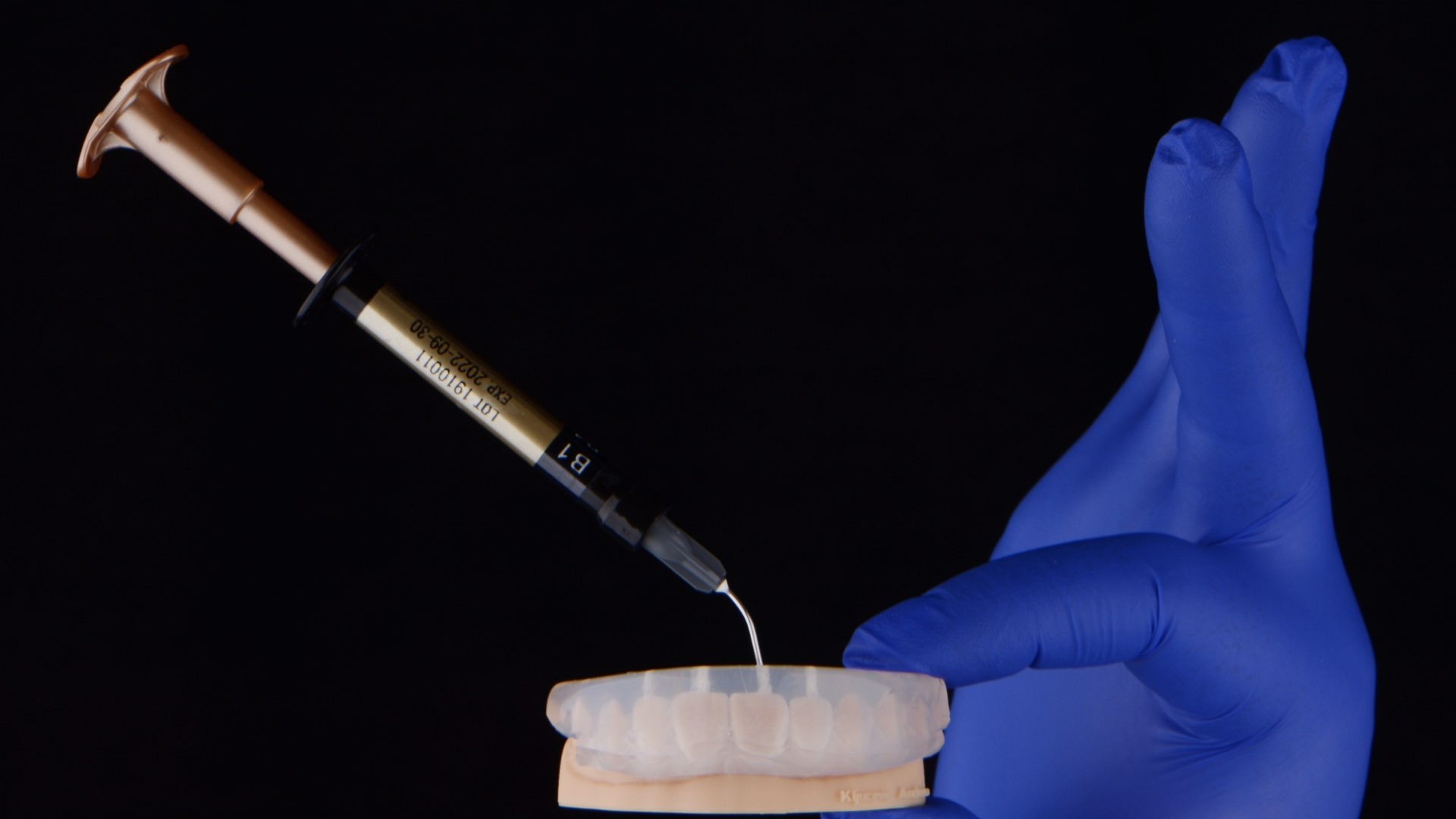
Composite injection protocol










Polishing and finishing
- Blade 12 for removing cervical and proximal excess
- Soflex disc for recontouring the proximal walls and thinning the cervical edge of composite
- Shofu One gloss for coarse polishing and creating the morphology – as well as removing the excess on palatal surfaces.
- High gloss – EVE twist polishers – red for matte surface, and beige for a nice glossy appearance.
- Proximal surfaces should be polished using polishing strips – This step should be done carefully to avoid creating diastemas again.



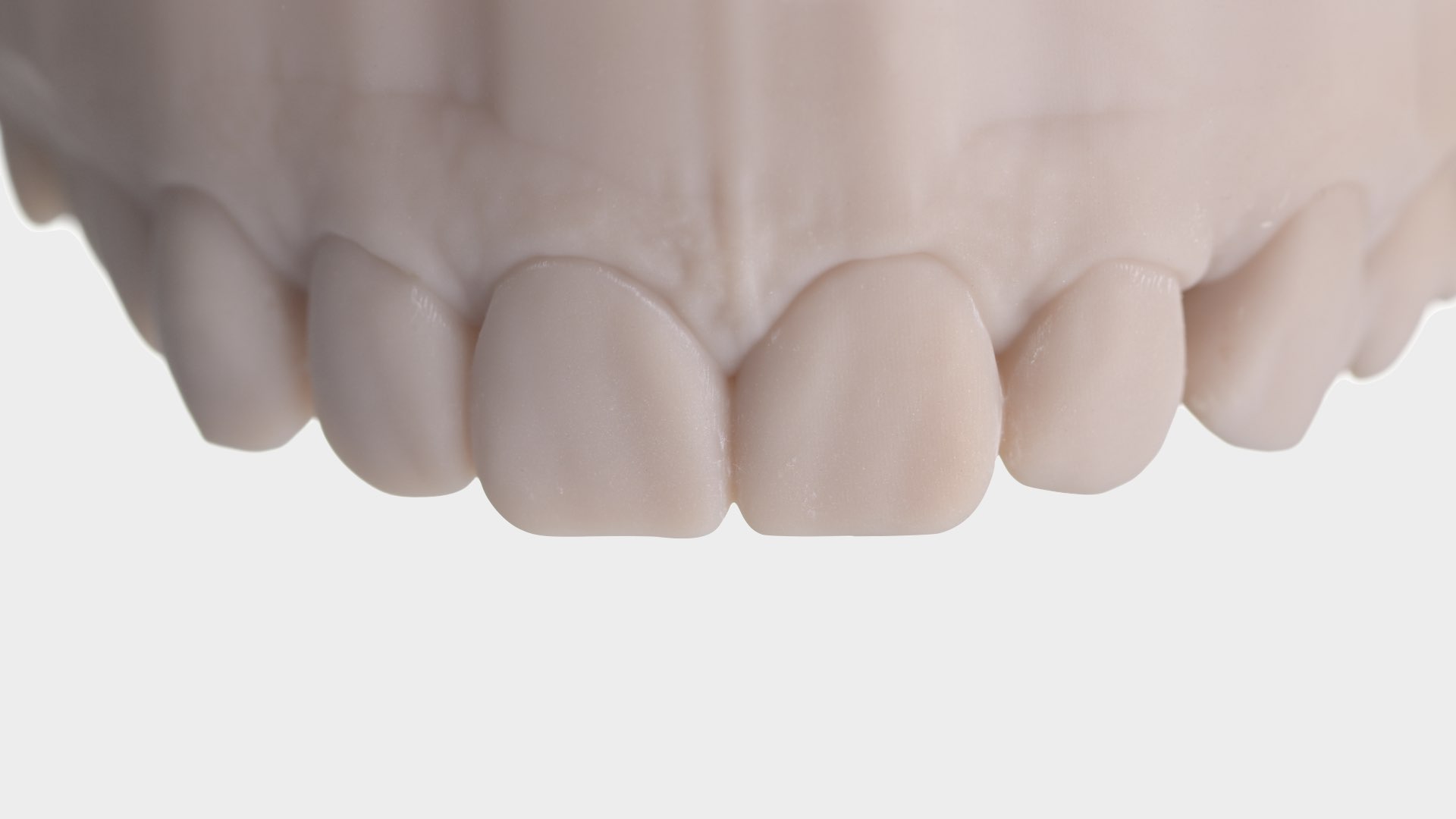
Final result

One day follow up


Designed vs. Delivered


Conclusion